MSS AI Study Group meeting on 18 March 2025
Summary of “Translating the Machine – The Use of AI in Medical Retina” by Professor Tariq Aslam
Professor Tariq Aslam, a leading figure in ophthalmology and technology research, explores the role of artificial intelligence (AI) in the subspecialty of medical retina—concerned with diseases of the retina, optic nerve, and macula, which are leading causes of vision loss in the Western world, including age-related macular degeneration and diabetic retinopathy.
Advanced imaging techniques such as optical coherence tomography (OCT), autofluorescence, and widefield imaging are central to retinal diagnosis and monitoring. These provide detailed views of structural changes, such as microaneurysms, pericyte loss, vessel occlusion, and neovascularisation, which inform treatments like injections, lasers, and oral or intravenous therapies.
Given the enormous volume of outpatient appointments in ophthalmology—7.5 million annually in England—AI offers promise in diagnosis, treatment prediction, and monitoring. Machine learning models can identify retinal biomarkers and predict disease progression, as seen in several studies targeting geographic atrophy. AI also aids patient engagement via tailored information delivery and record management.
Real-world AI tools such as Retmarker DR, Notal Home OCT, and RetinAI Discovery are used to detect disease progression, quantify retinal fluid, and support treatment decisions. AI has demonstrated high accuracy in specific tasks, sometimes rivalling expert clinicians. However, real-world deployment faces significant challenges: data dependency, interpretability, integration into clinical workflows, and infrastructural requirements such as computing power and regulatory oversight.
Professor Aslam discusses the AI development pipeline, which includes defining clinical challenges, data refinement, algorithm development, prospective trials, regulatory approval, and clinical integration. Key barriers include a lack of transparency, insufficient integration with existing knowledge, contextual limitations, and ethical concerns regarding autonomy and liability.
AI systems must be thoroughly validated for specific patient scenarios. Human oversight remains essential, particularly in areas AI struggles with—such as social context, empathy, and communication. Real-world examples illustrate that while AI may assist in decisions (e.g., identifying macular oedema as a chemotherapy complication), human judgment is required to interpret confidence levels and rationales behind algorithmic recommendations.
Professor Aslam emphasizes the importance of combining AI with human skills to optimize care, cautioning against over-reliance. He also notes that poorly implemented technology, such as certain electronic medical record systems, can increase clinician burnout and undermine patient care. Adoption of AI should be gradual, well-audited, and focused on augmenting—not replacing—clinical expertise.
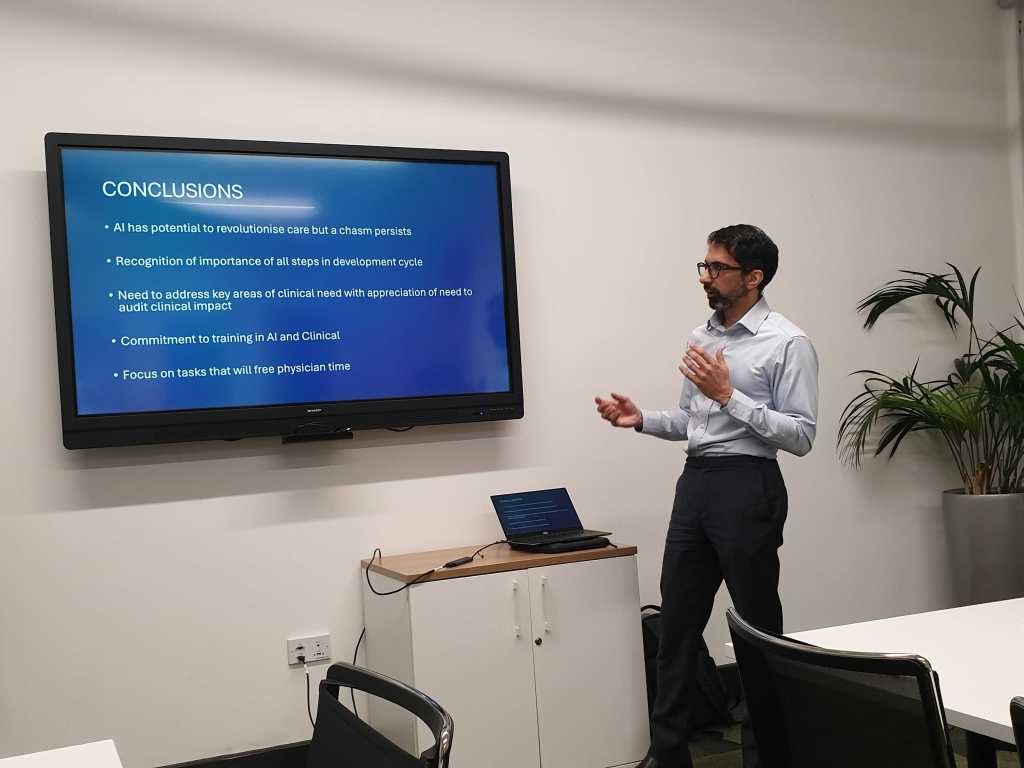
In conclusion, AI holds transformative potential in medical retina, but its successful implementation depends on thoughtful integration, training, and maintaining the human connection in healthcare. As Aslam and others argue, the true value of AI lies not in replacing doctors, but in restoring time for compassionate, patient-centred care.




Write-up created with assistance from ChatGPT.
